#14: How many people die from snakebites?
This week: Missing data – the most underrated problem in global health.
This is my fourteenth post of Scientific Discovery, a weekly newsletter where I’ll share great new scientific research that you may have missed. Check out the About page if you’re interested in why I’m writing this.
This week’s post is about what I believe is the most underrated problem in global health: missing data. But to illustrate it, I’m going to tell you about snakebites.
If you like this, I hope you subscribe! And if you spot any errors, please let me know so I can fix them.
How many people die from snakebites?
Here’s a statistic that might surprise you: Around 1 in 270 people in India die from snakebites by the age of 70.
In total, around 50,000 to 60,000 people in India die from snakebites each year. In Australia, which is home to the most-venomous snakes in the world, that number is 2. Just two.
Many more people live in India than Australia, so here’s another comparison. In India, the death rate from snakebites is around 5 per 100,000 people per year. In Australia, it’s 0.13, about thirty-eight times lower.12
If you aren’t from India, these statistics are probably new to you. But they are also surprising to many people from the country.
Deaths from snakebites are highly ‘spatially concentrated’. In urban areas of India, many people won’t know anyone who’s died from a snakebite. But in poor agricultural areas, many will.
Why do so many people die from snakebites in India?
Because snakebite deaths are caused by snakes and poverty together. Snakes are more common in places with grain agriculture, at low altitudes, where snakes live and feed on rodents and amphibians.
People who die from snakebites tend to live in poor rural parts of these areas, often work in farms, and lack access to hospitals, doctors and treatment.
Antivenom
Snakebites have a treatment: antivenom. But it might surprise you to learn that antivenom still comes from a method that hasn’t changed much in over a hundred years.3
First, venom is milked from the fangs of venomous snakes. Then, it’s injected into horses or other big animals. They produce antibodies to it, and these are extracted from their blood and purified into antivenom for humans.

Recently, there’s been an increase in research funding to create synthetic antivenom. But experts believe this isn’t enough, or isn’t happening fast enough: the current timescale when these might be available is thought to be 10–30 years away.
Current-day antivenom is very expensive. It’s also difficult to store and transport.
Here’s an excerpt by Mathias Kirk Bonde on the topic, in his excellent piece Advancing antivenom:
For over 34% of Indian snakebite victims, it takes more than six hours to receive treatment. If the clinic lacks a cold chain – a coordinated system of temperature-controlled environments – it is limited to using antivenom that can survive room-temperature storage. Without equipment to diagnose the species of snake the patient was bitten by, doctors must use polyvalent antivenom designed to work against multiple species of snake, which is typically more expensive and less effective than species-specific monovalent antivenoms.
Antivenom is no miracle cure and adverse immune reactions to it are common. Patients need to be monitored for up to multiple weeks after receiving antivenom in case of delayed serum sickness, which can be fatal.
In India, snakebite deaths happen more often in summers and during monsoon seasons. This is when more people are involved in agriculture, and when water floods into underground burrows and snake habitats. This leads them up into higher ground and buildings, and into contact with humans.
The flooding and disruption from monsoons is also likely to mean life-saving antivenom is even further out of reach for victims.

Even so, 50,000 to 60,000 snakebite deaths in India each year is a big number.
Only about 1,000 snakebite deaths are recorded per year by the Indian government.4 In 2008, a meta-analysis estimated around 11,000 deaths per year instead, based on how many people took insurance claims from a government scheme.
Well, this revised estimate was 58x the recorded number, and 5x the second estimate which was meant to capture underrecording.
Why were they so far off?
Missing deaths
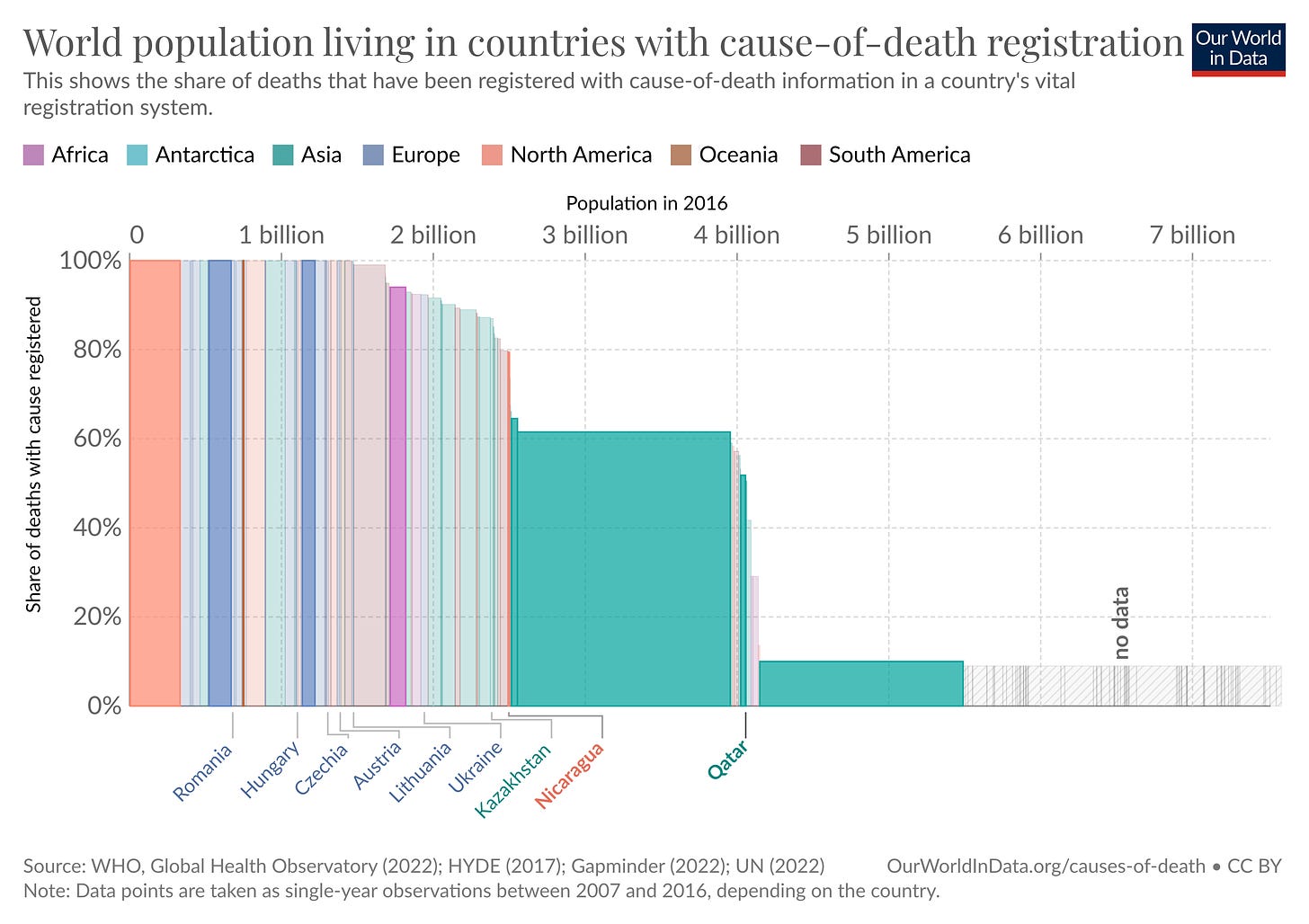
We take it for granted in much of the world that we know how many people are dying each year, and what they are dying from.
But that’s not the case worldwide.

In many countries, there isn’t a functioning civil registry, where births and deaths are regularly recorded. This means many deaths aren’t registered officially with a death certificate. But even among the deaths that are registered, many lack a ‘cause of death’ on the certificate.
In 2015, when it was estimated that around 56 million deaths occurred worldwide, only around half were registered with a cause of death.
Only around a fifth of all deaths worldwide in 2015 were reported to the WHO with a meaningful cause of death – which excludes ambiguous causes like ‘sudden death’, ‘chest pain’, ‘event of undetermined intent’ and others.
Missing deaths are common in poorer countries because of poorly functioning civil registries, because many people die outside of hospitals, because many don’t have medical records, because many lack a doctor or nurse to fill in their death certificate, and because many countries lack coroners to investigate unexpected deaths.
Because official records are limited, estimating the number of deaths from each cause can sometimes be difficult. In fact, the problem has several layers:
First, the cause of death is not recorded for many deaths.
People who die outside of hospitals are even less likely to have their deaths recorded.
They tend to die from different causes, because they have different demographics and different risk factors.
And finally, hospitals affect whether people die, and what they die from.

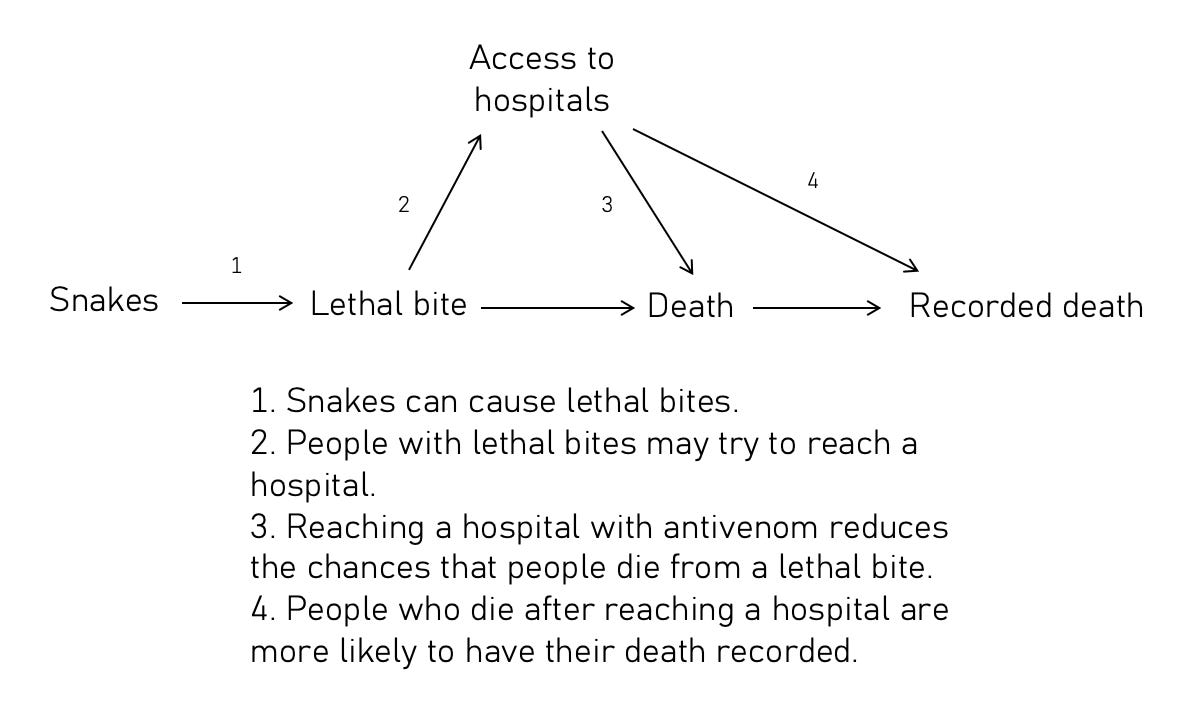
In India, around 94% of snakebite deaths occurred in rural areas, and 77% occurred out of hospital. This is why the previous estimates were so far off.
People who died from snakebites in these areas didn’t just lack access to the cure – they also lacked their deaths being counted.
This doesn’t mean we’re completely in the dark about what people are dying from around the world. Sometimes, data is available from some regions within a country, or from estimates from separate one-off studies.
But it means our understanding is often incomplete and irregular, and sometimes inaccurate. Missing deaths are a tragedy that I think don’t get the attention they deserve, and snakebite deaths are a dramatic example of it.
The Million Death Study
So where are the numbers in my post coming from? How were these revised estimates made?
Rather than using death records from hospitals (which we’ve seen are limited for causes of death nationally), they come from a national study in India called the Million Death Study. This was an important study because it deliberately collected data that had been missing.
It involved structured interviews of 1.4 million households across urban and rural areas of the country, every six months over a period of 15 years, about their relatives who died and the symptoms they had before their death. This method is called a ‘verbal autopsy’.
These households came from a random selection of thousands of small areas across the country, such as villages or urban blocks of about a thousand people each. The study was also inexpensive, with a budget of 2 million US dollars per year (about $1 per household).5
People’s answers to the interviews in the study were then coded into causes of death by multiple medical doctors, for each death. For snakebite deaths, they agreed on the cause of death about 92% of the time.
What are the limitations of this study?
When I read research, I try to imagine myself as a participant. What might make it more difficult for researchers to interpret the data they get from me?
In this case, the study involves interviewing relatives, so what comes to mind is: if I didn’t know or remember the symptoms before the person’s death. Or if the person who died didn’t have medical records or testing for diseases. These problems might make doctors misdiagnose the cause of death from my answers, especially if the symptoms I describe are shared with many other causes.
But that’s much less of a problem for deaths caused by injuries like snakebites, which are noticeable and often happen shortly before a death, making them memorable and easier to attribute.
On the other hand, when snakebites cause long-term complications that eventually lead to a death, those deaths could be harder to correctly attribute to snakebites, which suggests they may be underestimated.
As the study continued over a long period, we also have an idea of how death rates changed over time. For example, they found large declines in child mortality overall.
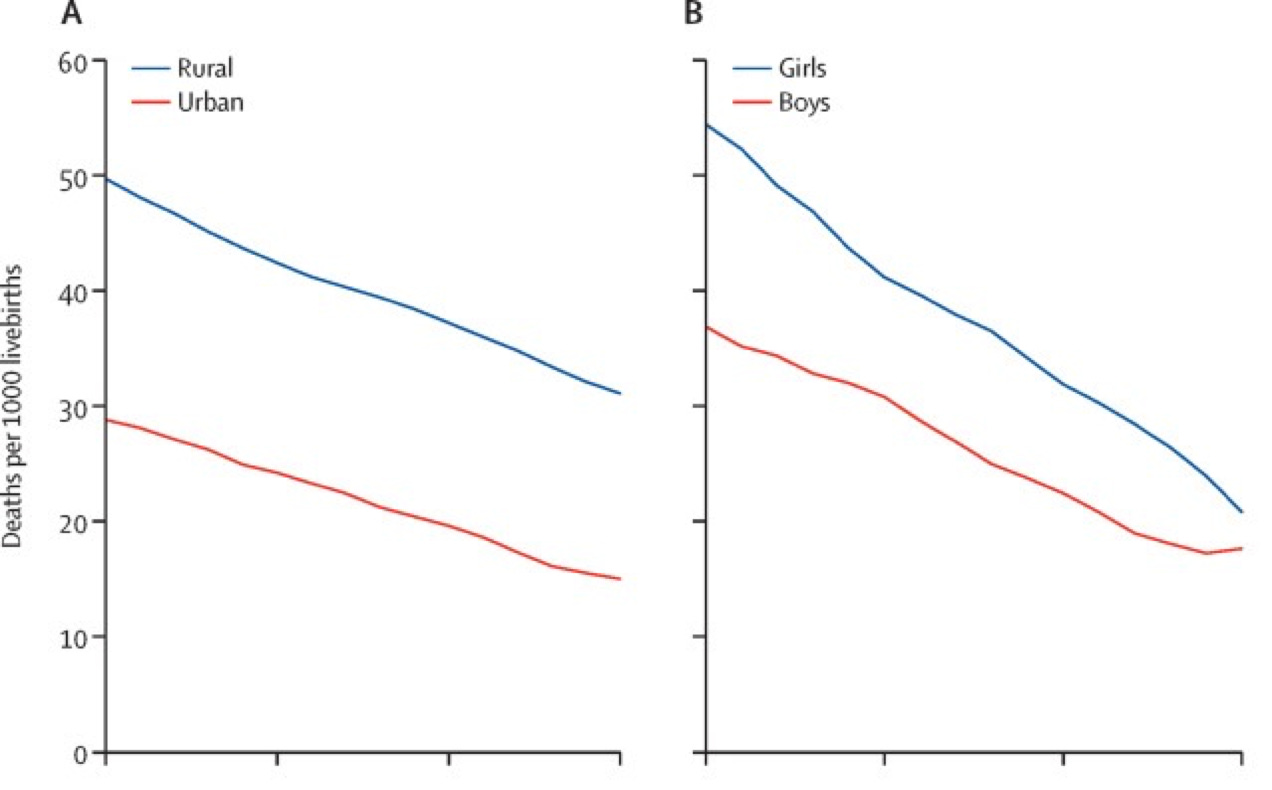
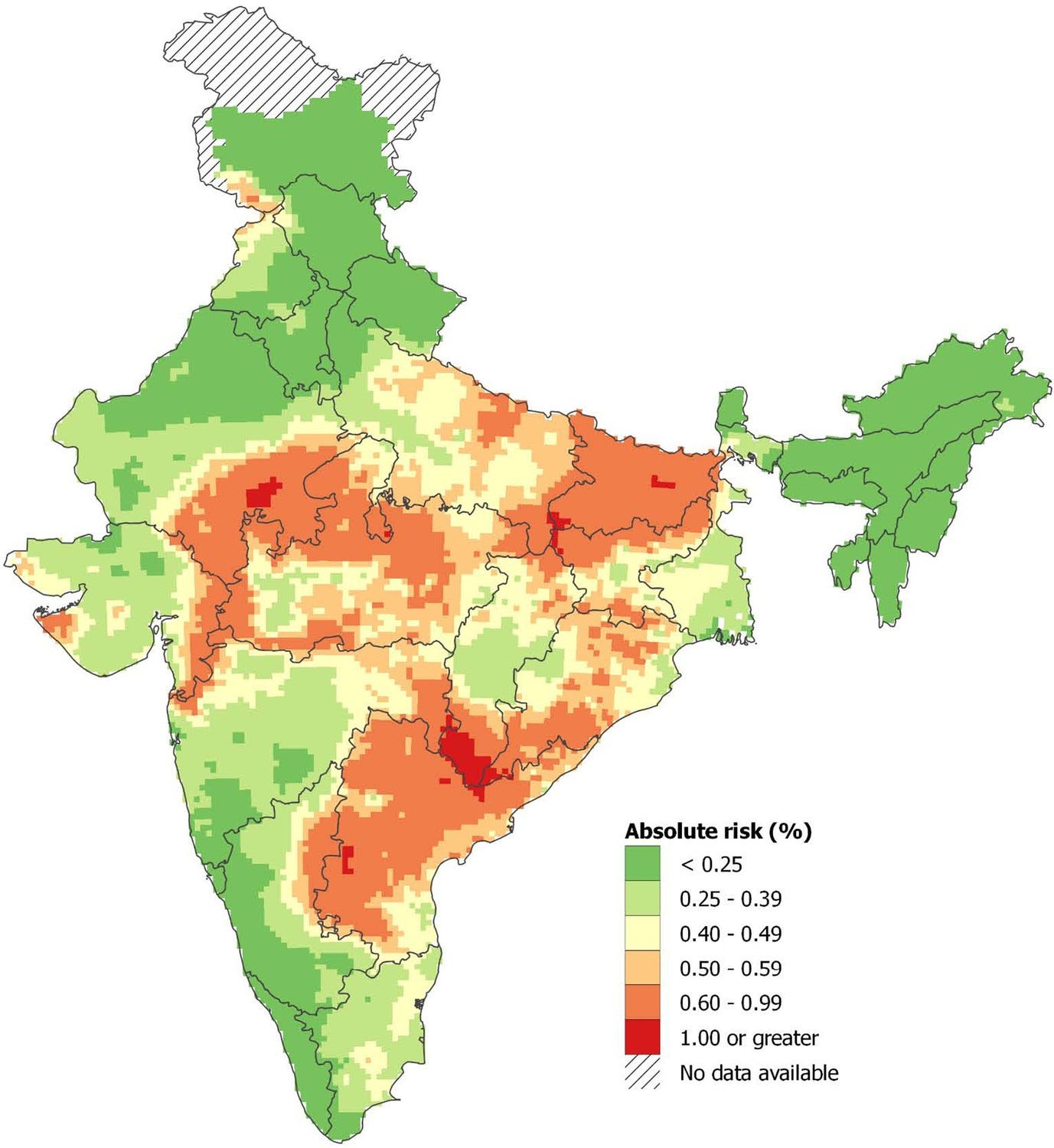
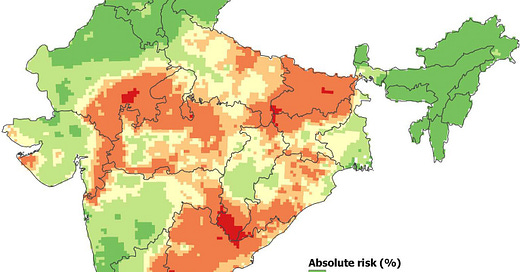
Snakebite death rates declined nationwide as well, and the absolute risk of dying from snakebite in India by the age of 70 declined from 0.4% to 0.37% between 2001 and 2014.6
But the changes varied between states: In the states that initially had a higher burden, the death rates slightly worsened (you can see this below).

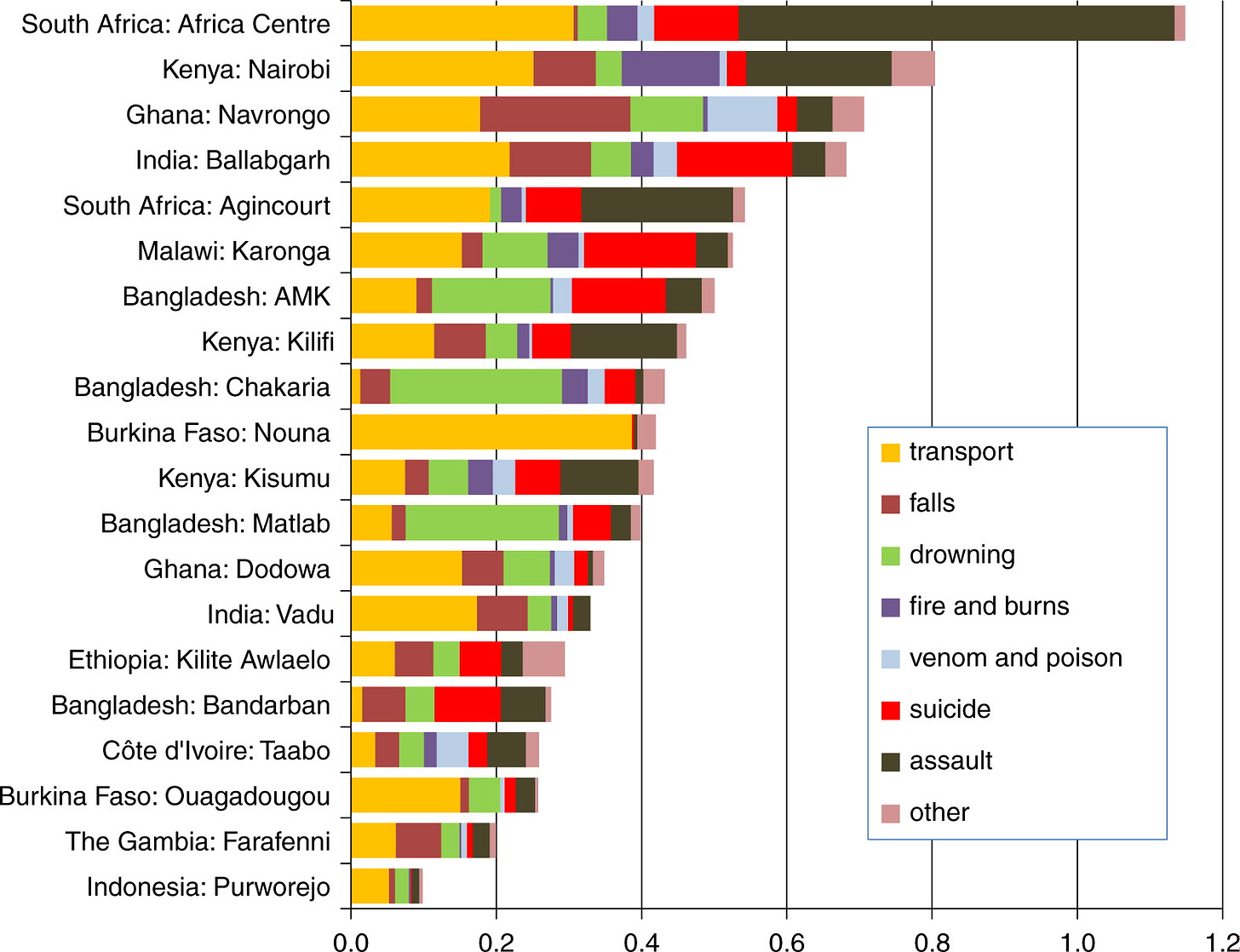
What about in other countries? Here’s a chart showing mortality rates from a range of external causes including venom, in a large verbal autopsy project that was conducted across 20 sites in Africa and Asia.
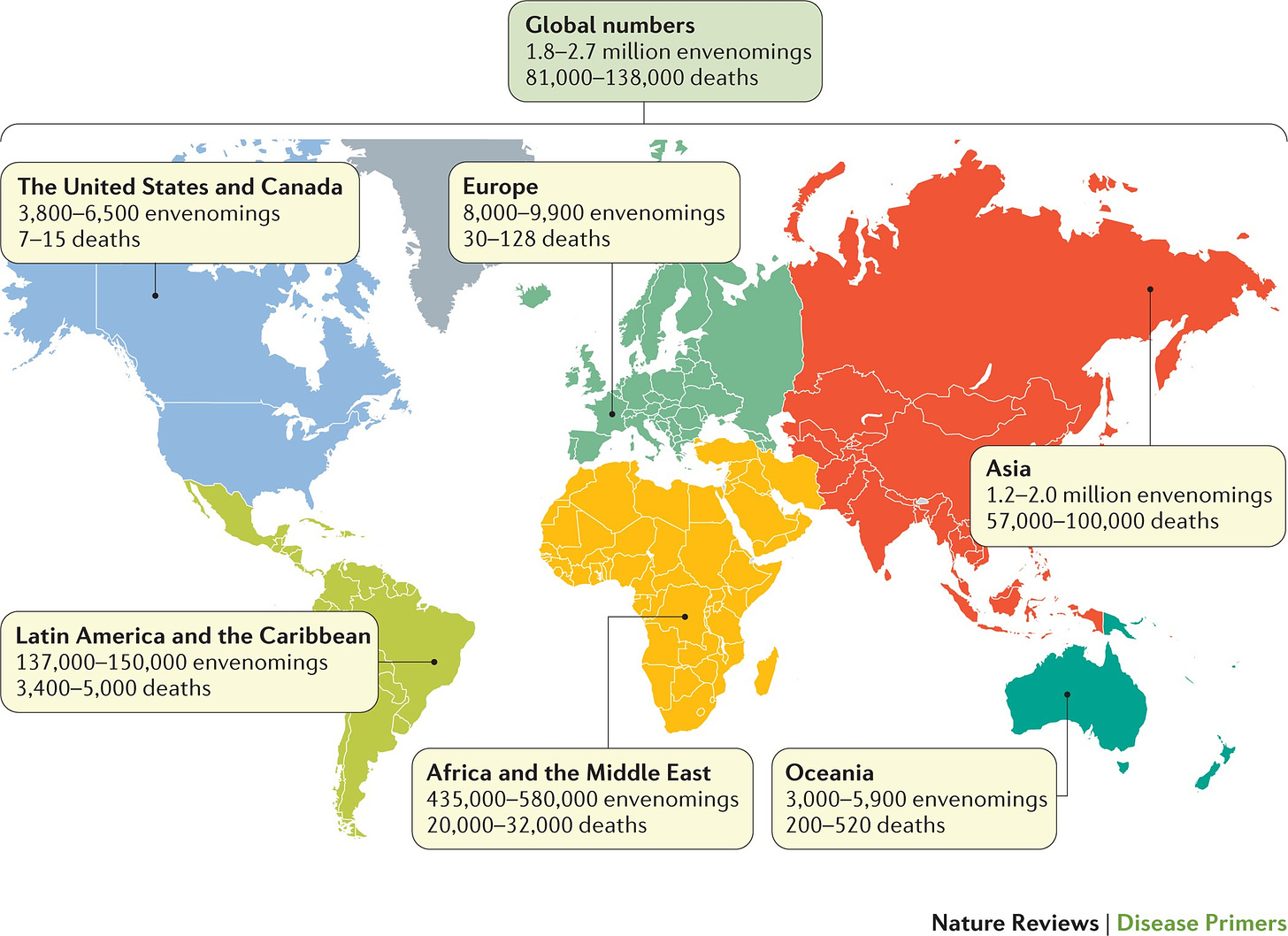
Because of these studies and others, the WHO now estimates that a total of 4.5 to 5.4 million people get bitten by snakes per year; that 1.8 to 2.7 million people develop illness from it, and that 81,000 to 138,000 die from its complications worldwide each year.7
Snakebite deaths are not a typical example, but they help to illustrate the challenge of missing data – how it arises, and how it can affect our understanding of big problems that affect people around the world.
I think missing data is one of the most, if not the most, underrated problems in global health. It doesn’t mean we’re completely in the dark, and it’s not an excuse to not act. But knowing precisely and accurately what people are dying from matters.
It helps put many other numbers in context: To calculate numbers per capita, rates per 100,000 people, percentages, and more. It’s essential in planning and decision-making, whether that’s by governments, NGOs, private companies, or individual people making decisions about their lives.
It helps us answer questions like: Which conditions are going untreated? Where are doctors needed? How many doses of medicines and vaccines are needed? How much progress are we making? Are new problems emerging?
By highlighting what we don’t know, we can bring attention to areas where more data and research would help the most. This is one of them.
I hope you liked this, learnt something new and subscribed if you haven’t already! I’ve double-checked and sometimes triple-checked most of the numbers, but if you spot anything I’ve gotten wrong, please let me know.
Links
If you’re interested in more on this topic, here’s some recommended reading:
The lifesaving power of … paperwork? – a piece on the importance of death registration around the world, by Jeneen Interlandi at the New York Times.
Advancing antivenom – a piece on the past, present and future of antivenom, by Mathias Kirk Bonde at Works in Progress.
Snakebite data information portal – where in the world do snakes live? The WHO has a new data portal with lots of maps about this.
The tale of snakebite’s fleeting spotlight—and why it encapsulates all that’s wrong with global health – by Robert Fortner in the BMJ.
Challenges and prospects of snake antivenom supply in sub-Saharan Africa – by Abdulrazaq G. Habib et al., in PLOS Neglected Tropical Diseases.
Snakebite – a summary of the Wellcome Trust’s research funding projects on developing new antivenom.
That’s all for now! I’m sorry my posts haven’t been regular – I started this newsletter hoping to publish posts once a week, but with all my other work I’ve had to choose between speed and quality, and I’m prioritising the latter.
Hopefully I’ll find ways to do both better in the future.
See you next time :)
– Saloni
Updated 13/04/2023: I replaced the case-fatality rate in the text with the death rate, because there was more uncertainty over the number of cases in Australia, which meant the case-fatality rate was less clear. (The case fatality rates: In India, the chances of dying after a venomous snakebite are about 3.8%. In Australia, the chances are 0.06% with 2 deaths and around 3000 venomous bites each year, about sixty times lower, but the number of bites seems to be a fairly rough estimate.) I’m sorry about this!
Note the uncertainty is relatively wider for the rates in Australia because of the very low absolute number of deaths.
The recorded number of snakebite deaths from the Central Bureau of Health Intelligence in India: 1,124 in 2006, 1,299 in 2007, 1,364 in 2008; 1,068 in 2016 and 1,060 in 2017.
Updated 11/04/2023: I made a mistake here in the original version of this post and said this was the total budget. It was actually the per-year budget, and I’ve now corrected this. Thank you to Otis Reid for pointing it out!
In other words, they declined from an absolute risk of 1 in 250 people to 1 in 270, by the age of 70, between 2001 and 2014. Or using another metric, the mortality rate, they declined from 5.3 to 4.7 deaths per 100,000 people per year.
Updated 12/04/2023: I added a map showing revised estimates of snakebite deaths worldwide. It’s important to note the lack of data coverage is still a problem in many countries, especially in Africa and Asia.



Most interesting article I've read this month. Is the lower p(death|snakebite) in Australia simply due to greater access to antivenom meds? Are the numbers for Australia adjusted for underreporting like the #s for India?
Really interesting article. Thank you so much saloni. My family lives in an area outside Bangalore very close to agricultural fields and often spot snakes, cobras especially.
Often wondered about the statistics around snakebites. Learnt a lot from your post